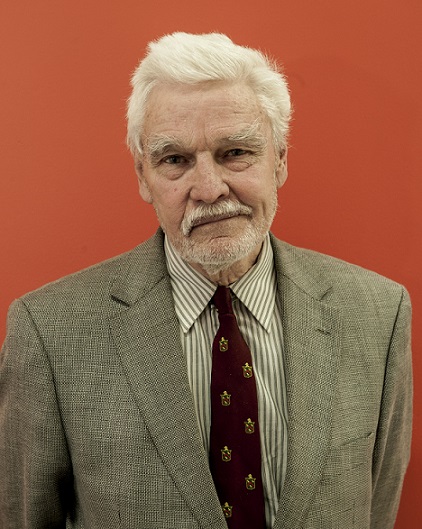
THE following address was given by Dr Rodney Syme, Vice President of Dying With Dignity Victoria, to the 2015 Annual General Meeting of the Rationalist Society of Australia.
Although I am nearly 80 years old and retired from surgery, I am still practising medicine. For over 25 years I have been counselling people about their end of life concerns. Those conversations are prolonged and open ended. At all times, I endeavour to help people to go as far with their lives as possible. From that experience I have learnt one invaluable lesson – my first self-evident truth – that giving people control over the end of their lives is one of the most valuable tools we have at our disposal.
This evening I am going to address the gap between the rhetoric and the reality of palliative care.
From humble beginnings, due to the compassion and energy of Cicely Saunders, palliative care has grown from a single London hospice to a world-wide specialty with strong government support. It is one of the most important developments in modern medicine. It aims to provide compassionate and holistic care for the terminally ill.
Examination of at least 27 journals devoted to research into palliative care reveals an intuitively obvious conclusion – that ethical research in this area is fraught by a constantly moving target making accurate statistical analysis virtually impossible. Despite the subjective impression that most patients benefit from their hospice care, it has been exceedingly difficult to demonstrate any objective benefits for such care. Yet this sheer volume of research gives an appearance of scientific validity to the specialty. We constantly hear of the tremendous advances in palliative care. Governments constantly say that there is no need to revise laws on assisted dying because palliative care deals with all those problems very effectively.
What is the response from palliative care to this rhetoric? Only to confirm that it deals very effectively with pain in the terminal patient. There is no public discussion of how this terminal pain, or other suffering, is relieved. It consistently evades any public discussion of other aspects of suffering.
There is no public discussion of how this terminal pain, or other suffering, is relieved. It consistently evades any public discussion of other aspects of suffering.
Careful examination of this literature reveals the extent of suffering in the terminally ill, and the difficulty in measuring and relieving it. The inordinate focus on the successful relief of pain is contested by Professor Michael Cousins, who in 2010 stated that “10% of cancer pain was so difficult to treat at the end of life that some patients were given drugs to sedate them to unconsciousness, culminating in death over several days to a week.” But breathlessness, cachexia (wasting, weakness, immobility and dependence), anorexia, nausea and vomiting, incontinence, ulceration, discharge and odour are common and far more difficult to palliate, and all impact on dignity. And this does not begin to address psychological, social and existential suffering, described by Francis Norwood as “social death”.
Is it surprising that palliative care does not entirely succeed with the palliation of suffering? Not at all. It is a monumental task, when you consider these further self-evident truths:
- First, that intolerable and unrelievable suffering is common in terminally ill persons, and often escalates as death approaches;
- Second, that some suffering is only relieved by death.
It is an especially difficult task when you maintain, as a matter of integral philosophy, that palliative care does not hasten death; and you are battling a constantly accelerating target, using a relatively poor tool kit. As evidence of the latter, let me cite a recent paper:
“Patients receiving palliative care are at high risk of adverse effects from drugs. As these effects can be difficult to distinguish from the symptoms of the terminal illness, harm from medicines is often not recognised. Adverse effects contribute to the burden of symptoms at a time when good control of symptoms is paramount. Adding another drug to treat the adverse effects can compound the problem.”
This paper effectively indicates that even 50 years after the establishment of palliative care, a level of experimentation goes on in treating terminally ill patients.
Palliative Care Australia acknowledged in 2008 that it could not relieve all pain and suffering, even with optimal care, but it was being a little disingenuous because it did not disclose its trump card, terminal sedation. In the 1980s the Graseby pump was developed and Midazolam became available, compatible with morphine in a common syringe. First reported in 1988 for ‘terminal restlessness’, terminal sedation was described as providing “a readily available means of controlling symptoms and overcoming patient distress where no feasible alternative existed previously.” In 1990, Ventafridda reported its use in 52% of palliative outpatients, to howls of anguish from others who stated they never, or very rarely, did so. Billings and Block described it as “slow euthanasia” to more howls of dissent. They famously defined slow euthanasia as “the clinical practice of treating a terminally ill patient in a fashion that will assuredly lead to a comfortable death, but not too quickly”, and included terminal sedation in this definition. They were challenging the soft defence of intention, and focusing on outcome. They also asked “Why should a patient who requests a quick death be subjected to a slow dying?”
Its use has subsequently expanded to refractory pain, breathlessness, extreme fatigue, psychological and existential distress. It is very clear that palliative care has the tools to relieve any intolerable suffering, but I have never heard or seen this made evident to the public. It remains the Achilles heel of palliative care because it is used in exactly those circumstances where other doctors might provide assisted dying if they were asked. And this very process is only associated with patient consent in up to 50% of deaths, with no opportunity to say goodbye.
It is very clear that palliative care has the tools to relieve any intolerable suffering, but I have never heard or seen this made evident to the public. It remains the Achilles heel of palliative care because it is used in exactly those circumstances where other doctors might provide assisted dying if they were asked. And this very process is only associated with patient consent in up to 50% of deaths, with no opportunity to say goodbye.
Far from acknowledging terminal sedation, palliative care has been assiduously arguing that neither it nor morphine alone, if used in a proper palliative way, ever hastens death. Terminal sedation is justified for the treatment of ‘refractory’ or ‘intractable’ symptoms, as determined by the clinician, not the patient. “Despite the huge progress made in palliative medicine in terms of symptom control, many are intractable symptoms, either because the treatment is ineffective or because the treatment itself is intolerable.”
However, in order to demonstrate that hastening of death is not the intention, the treatment is slowly titrated to a level where consciousness is suppressed, and, in association with withdrawal of hydration, death inevitably follows. I would have thought that if symptoms were intractable, and death clearly imminent, there would be an imperative to provide maximal relief of any pain and suffering as soon as possible. But no, even though in law there is no problem with hastening death if the intent is to relieve suffering (Devlin in R v Adams, Victorian Medical Treatment Act), titration is obligatory under the ‘palliative model of care’ – suffering continues until unconsciousness ensues, which may take days. And this occurs despite senior consultant Robert Twycross stating “nothing short of deep unconsciousness could provide relief and … inadequate sedation makes matters worse.” For a profound analysis of terminal sedation read Prof Erich Loewy who wrote “Terminal sedation, we would claim, differs from some form of voluntary active euthanasia mainly in that it has not been and is unlikely to be legally challenged.”
Despite the availability of terminal sedation, eminent British geriatrician and ethicist Professor Raymond Tallis reports the opinion of a PC physician that 15% of deaths are ‘bad deaths’ – and that is the opinion of the doctor, not the patient. In a Lancet Editorial Janet Hardy wrote “the concept of sedation causes considerable unease in many palliative care workers, most of whom are ardently opposed to any form of euthanasia or patient-assisted suicide. There is concern that sedation as the best means of symptom control in the dying patient is underused because of fear of employing terminal sedation.”
Palliative Care Australia acknowledges that patients do make rational and persistent requests for a hastened death: Roger Hunt found 25% of his PC patients did so. Yet “the view of a prominent segment of the palliative care professional community … almost without exception … [is] that patients who receive state-of-the-art palliative care, including psychosocial and spiritual interventions, almost invariably cease and desist from their desire for a hastened death.” Surprising? No – who has all the power in such discussions? Could this not be seen as duress?
The inherent ‘goodness’ of the enterprise, and the essentially closed nature of hospice, has allowed the rhetoric of palliative care to escape examination. As palliative care specialist Derek Doyle wrote, “a metaphorical halo shines over specialist palliative care and its practitioners with the result that some of its claims and assumptions have gone unchallenged by all but a few.”
Palliative care specialist Fiona Randall is one of those few.
She describes “the inflated and often contradictory claims made in the literature of palliative care – its rhetoric … which cannot, in reality, be enacted in clinical practice.” The language of palliative care offers an “impeccable” assessment and treatment of pain and other symptoms and “exquisite” and “meticulous” nursing care. Randall says, “This is embarrassing rhetoric … Palliative medicine claims to alleviate emotional, psychological, social and spiritual suffering, in addition to physical symptoms. There is no other speciality which claims to do all these.
“Moreover, palliative medicine claims to be able to alleviate these forms of distress and improve quality of life, even in the context of dying. Dying is generally perceived to be associated with great distress, yet in palliative care it is held that we can apparently achieve relief of symptoms, including those of a psychosocial and spiritual nature.
“The goal of impeccable relief of pain and other symptoms is unachievable, and the expectations generated by the philosophy statement are unrealistic. Setting unachievable goals for one set of people and promoting unrealistic expectations which will not be met in another group of people is unfair to both and likely to lead to harm for both.”
Ben Rich stated in 2014 that “Others have raised concerns about an authoritarian streak, or a form of hard paternalism, in the philosophy and practice of hospice. Those concerns denote a perception that some in the hospice movement maintain a rigid and monolithic view of death: one size fits all – it’s the hospice way or the highway.”
“Others have raised concerns about an authoritarian streak, or a form of hard paternalism, in the philosophy and practice of hospice. Those concerns denote a perception that some in the hospice movement maintain a rigid and monolithic view of death: one size fits all – it’s the hospice way or the highway.”
Sociologist Julia Lawton, who was embedded in British palliative care for 10 months, wrote “The research highlights the difficulties of matching the modern hospice movement’s ideological goal of enabling patients to ‘live until they die’ with the realities of the ways in which many patients, cared for in hospices, bodily degenerate in practice.”
Palliative care has been described as a model of care which has become more and more defined and specialized, into which the patient must fit. The Liverpool Care Pathway was an example of such a model, but failed because it did not treat people as individuals and ask what care they wanted. It led to abuse of autonomy. We are all individuals, shaped by our own experience and values. For government to suggest that we should all fit into a specific model of care is extraordinary.
Religion – the Elephant in the Room
Ian Maddocks, the first Australian Professor of Palliative Medicine, states that “The roots of modern palliative care are of course to be found in religious orders concerned with the care of the dying” and that “Palliative care usually has adopted a confrontational position against voluntary euthanasia, partly because of the historical association with Christian (Catholic) concern to preserve life.”
Associate Prof. Alex Broom spent six months embedded in a Catholic hospice, interviewing doctors, nurses and patients. He found an atmosphere of tension, with death in the air, a place of unbounded and hopeless bodies. Patients had a sense of impotence; they were subdued within the hospice’s ideological frame, with a sense of entrapment.
He found among the patients virtually unanimous support for assisted dying, but the hospice was totally opposed. A desire for a hastened death was seen as a call for help; the patient ‘just needed more time’ to adjust, their request was met by spiritual and social support. The assessment was that it was ‘not his time to go.’ Assisted death was not part of hospice care, which had an ideological model of dying, based on religious contexts.
He also found an underlying Catholic influence in the hospice. Although it was a site of medical care, it had Christian underpinnings and an interplay of religiosity which was rarely explicitly acknowledged. The care was precariously placed between care of the body and care of the soul.
Cardinal George Pell proudly states that 57% of Australian palliative care is provided by the Catholic Church. There is no other area of Australian medical practice which is so infiltrated by a specific moral framework. There can be no doubt that the religious origins of palliative care and this religious dominance in its provision has a profound effect on how people die.
Palliative Medicine Professor Sam Ahmedzai, a critic of euthanasia but a supporter of assisted suicide, wrote, “It is patronising to say that a few people should suffer unbearable distress and indignity because palliative care preaches that it values all lives, regardless of how meaningless they have become to their owners. It is inconsistent for palliative care to boast how it enables people to face the reality of dying and decide about place of care but then to deny choice for timing of death. Moreover, it is hypocritical to deny competent patients who are acknowledged to be dying the right to die in a manner of their choosing, while allowing doctors and nurses to place them on a so called care pathway, which often entails increasing sedation and withdrawing fluids, unintentionally leading to a protracted form of assisted dying, but one that is medically determined.”
Let us consider the above in the light of my final self-evident truths.
- First, that a doctor has a duty to relieve suffering. Sir William Osler wrote over 100 years ago that a doctor’s duty was to ‘ease death’.
- Second, that a doctor has a duty to respect his patient’s autonomy.
Given these fundamental ethical obligations, should a doctor, treating a patient with intolerable and unrelievable suffering who asks for assistance to die, simply offer refusal of treatment, or slowly progressive sedation, or the option of refusing food and fluids, as is suggested by the American Association of Hospice and Palliative Medicine?
Some people listening to me may think I am violently opposed to palliative care. Not so. I support open and frank communication between dying patient and doctor, supporting the patient to go as far with their life as possible, encouraging the acceptance of the reality of dying, maximal relief of pain and suffering, giving them a sense of control over the end of their lives, respecting patient autonomy and encouraging dialogue between the dying patient and their family with the important object of allowing them to say goodbye – all good palliative principles. But I do not accept the rigid imposition of a particular model of care, and a limited choice at the end of life which condemns some people to die in a way that is anathema to them, in order to satisfy the moral view of their doctor.